A single security gap jeopardizes millions of confidential patient histories, undermines carefully established credibility, and prompts severe financial sanctions from regulators. In the digital medical landscape, robust data security healthcare measures are the foundation of any application. The rapid expansion of mobile technology into the mentioned sphere has created a new frontier for patient care.
Applications now manage everything from sensitive diagnostic information to real-time treatment plans. This convenience, however, comes with immense responsibility. The core challenge for developers and organizations is navigating the complex web of healthcare IT compliance requirements.
In the digital age, a system vulnerability can become a matter of life and death, not merely a technical glitch. A failure in healthcare cybersecurity software can have consequences far beyond a typical data breach, directly impacting human well-being. This article will explore the unique threats facing medical applications and outline the definitive strategies for achieving resilience. We will dissect the major regulatory frameworks.
What makes healthcare apps unique in terms of security
Medical applications operate in a distinct category defined by the extreme sensitivity of the information they handle and the direct impact on human health. Unlike a social media or e-commerce platform, a breach here has tangible, real-world consequences. The distinctiveness originates directly from the inherent characteristics of the information involved. These platforms manage Protected Health Information (PHI), a comprehensive category that includes medical histories and treatment records, and also identifiers like names, contact details, and financial account numbers. Such a combination creates a highly attractive target for cybercriminals.
Furthermore, the ecosystem is inherently interconnected. A single mobile app must often communicate with hospital electronic health records (EHRs), laboratory systems, and insurance databases, creating multiple potential entry points for attacks. This complex web of integrations makes a unified healthcare data security software strategy essential. The stakes are simply higher, as a failure can lead to misdiagnosis, incorrect medication, or delayed care, moving beyond financial loss into the realm of patient safety.

Why security and compliance are critical in mobile healthcare apps
Understanding why data security is important in healthcare is the first step toward building trustworthy solutions. The imperative is twofold: ethical responsibility and legal obligation. From an ethical standpoint, patients entrust developers and providers with their most private details. Betraying that confidence through negligent data protection healthcare practices can cause significant personal harm and shatter the essential bond between individuals and the medical system.
From a legal perspective, the framework is exceptionally strict and offers little room for error. Binding regulations such as HIPAA and GDPR carry the force of law, imposing substantial monetary fines for any failures to adhere. These specific statutes require implementation of defined technical controls and procedural measures to guarantee the privacy, accuracy, and consistent accessibility of medical data. The mentioned rules mandate specific technical and administrative safeguards to ensure the confidentiality, integrity, and availability of health information. A robust approach to healthcare software compliance is also a powerful business asset.
All of the above builds market credibility, facilitates partnerships with major healthcare institutions, and provides a competitive edge in an industry where trust is the primary currency. For organizations looking to navigate this complex terrain, expert guidance is invaluable. Specialized firms offering healthcare app development and patient-centric app development can provide the necessary expertise to build a foundation of trust from the ground up.
“Data protection serves as healthcare’s fundamental currency of trust, determining both credibility and market longevity.”
Core healthcare IT compliance
Navigating the global regulatory environment is a fundamental task for any digital health initiative. Healthcare security compliance is a continuous journey of adhering to various overlapping frameworks. These regulations set the minimum standard for data protection in healthcare, dictating how information must be collected, stored, processed, and shared.
A comprehensive strategy often requires understanding and implementing controls from several different standards simultaneously, especially for applications targeting international markets. The following sections break down the most critical regulations that shape the industry today.
1. HIPAA (US)
HIPAA (Health Insurance Portability and Accountability Act) is the cornerstone of medical data security and healthcare regulation in the United States. Its Security Rule establishes national standards for protecting electronic PHI (e-PHI). Adherence to these standards is mandatory for all organizations handling protected health information, including medical practitioners, insurance carriers, and their contracted partners. The rule mandates safeguards in three key categories: administrative, physical, and technical.
Administrative controls involve risk analyses, staff training, and contingency planning. Physical measures govern access to hardware and facilities. Crucially, technical safeguards require specific healthcare cybersecurity software features, including access controls that grant system entry only to authorized users, encryption of e-PHI both at rest and in transit, and activity logs and audit controls to monitor system access.
2. GDPR (EU)
GDPR (General Data Protection Regulation) is a comprehensive EU law that applies to any organization processing the personal data of individuals within the Union, with a special classification for health information. While HIPAA focuses specifically on covered entities, GDPR’s scope is far broader. The framework codifies fundamental tenets, including “legal basis, equity, and openness” alongside “restriction of purpose.” For digital health solutions, this translates to securing unambiguous, well-understood user authorization prior to any information gathering and maintaining complete transparency regarding its intended application.
A core right under GDPR is data portability, allowing individuals to obtain and reuse their information across different services. The regulation also includes a stringent breach notification mandate, requiring organizations to inform authorities within 72 hours of becoming aware of an incident. The penalties for non-compliance can be severe, reaching up to 4% of annual global turnover. The official EU GDPR Portal serves as a critical resource for interpretation and implementation.
3. ISO Standards (27001 / 27799)
While government regulations are legally binding, International Organization for Standardization (ISO) guidelines represent internationally recognized best practices. The ISO 27001 standard outlines precise criteria for creating, deploying, and continuously operating an Information Security Management System (ISMS). This approach offers a methodical structure for safeguarding an organization's confidential data, maintaining its protection over time.
For the medical sector, ISO 27799 offers guidance specifically tailored to health informatics. It serves as a companion to ISO 27001, outlining controls and measures that are particularly effective for protecting patient data. Achieving certification against these standards demonstrates that an organization has implemented a world-class, verified security program. It is a powerful signal of commitment to healthcare security software excellence. The detailed specifications can be found in the ISO 27799 standard documentation.
4. PIPEDA (Canada)
Canada’s Personal Information Protection and Electronic Documents Act (PIPEDA) governs how private-sector organizations collect, use, and disclose personal information in the course of commercial business. It applies to health data collected in the context of commercial activity. PIPEDA is based on ten fair information principles, including accountability, identifying purposes, consent, and limiting collection.
Similar to GDPR, PIPEDA emphasizes individual access, allowing people to challenge the accuracy and completeness of their information. For application developers in the Canadian market, understanding the specifics of obtaining meaningful consent and implementing appropriate security safeguards is paramount. The Office of the Privacy Commissioner of Canada provides comprehensive resources and guidance on complying with this important legislation.
5. NHS (United Kingdom)
Developing digital tools for the United Kingdom’s National Health Service (NHS) involves meeting a rigorous set of standards beyond general GDPR compliance. The NHS has its own digital maturity assessment and compliance frameworks. This is the Data Security and Protection Toolkit, which all organizations handling NHS patient data must complete.
The mentioned standards ensure that software and platforms integrating with the NHS are secure, interoperable, and uphold the highest levels of data protection in healthcare. They cover areas like clinical safety, operational resilience, and cybersecurity. Adherence to these protocols is non-negotiable for any vendor operating within or alongside the UK’s public health system. Developers should always refer to the latest guidelines on the official NHS website.
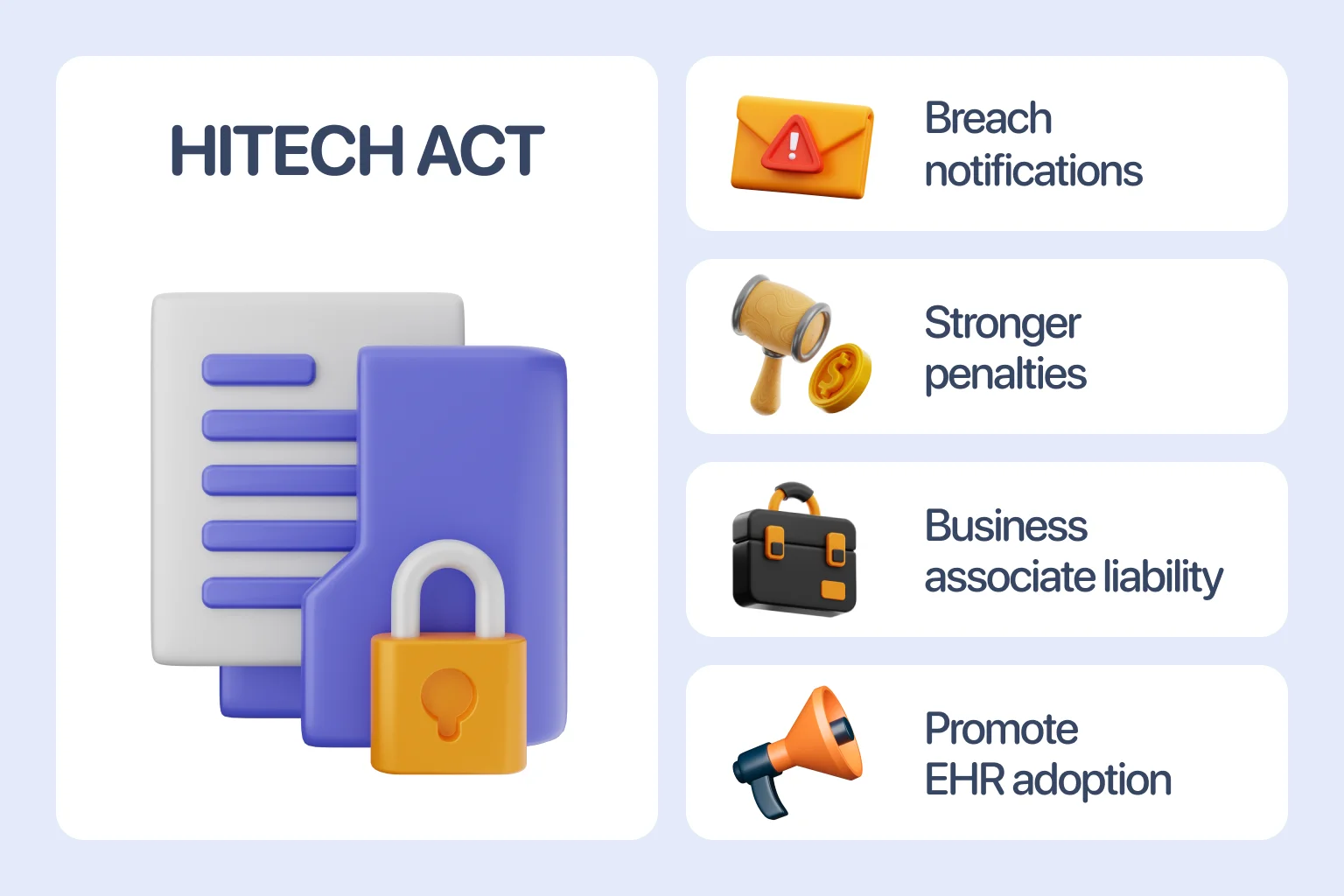
6. HITECH
The Health Information Technology for Economic and Clinical Health (HITECH) Act significantly strengthened HIPAA enforcement and expanded its scope. Enacted to promote the adoption of electronic health records, HITECH introduced stricter penalties for violations and established mandatory breach notification requirements for unsecured protected health information.
It also extended HIPAA’s obligations directly to the business associates of covered entities, making healthcare IT compliance a shared responsibility across the entire service chain. This act was a pivotal moment that increased accountability and incentivized robust healthcare cybersecurity software implementation. A detailed overview of its provisions is available on resources like the HITECH Act Wikipedia page.
Biggest data security threats for mobile health apps
Recognizing prevalent security gaps establishes the essential foundation for constructing robust protection mechanisms. The mobile ecosystem introduces distinct obstacles that demand tailored safeguarding approaches.
Let’s examine the primary dangers in detail:
- Insecure APIs & data transmission.
Application Programming Interfaces are the backbone of functionality, enabling communication between an app and servers. If these interfaces are not properly secured, they become a prime vector for threat actors. Weak authentication, insufficient rate limiting, and a failure to encrypt data in transit can expose vast amounts of sensitive information.
- Device-level risks.
Unlike controlled server environments, mobile devices operate in the wild. They can be lost, stolen, or run on compromised operating systems with outdated security patches. Malicious software on a user’s phone can also intercept data entered into or displayed by an otherwise secure application.
- Reverse engineering & code tampering.
Attackers can deconstruct an app’s code to discover hidden vulnerabilities, steal intellectual property, or even create malicious clones. Without proper obfuscation and integrity checks, a mobile app can be tampered with to bypass security controls or inject malicious code.
- Insider and cloud misconfigurations.
Not all dangers are external. Human error remains a significant factor, whether through accidental data exposure by an employee or, more seriously, the incorrect configuration of cloud storage services.
Publicly accessible databases containing unencrypted patient records are a sadly common headline. Proper architecture is critical, which is why many teams leverage expert cloud application development services to build a secure foundation.
Penalties & consequences of non-compliance
Failing to meet healthcare security compliance standards carries severe repercussions that can cripple an organization. The most immediate impact is financial. Regulatory bodies have the authority to levy multi-million dollar fines for violations. For instance, HIPAA penalties can reach $1.5 million per year for identical provision violations, while GDPR fines can be up to €20 million or 4% of global annual revenue, whichever is higher.
Apart from monetary sanctions, institutions confront expensive litigation processes, encompassing collective legal claims initiated by impacted parties. The harm to an organization’s public standing frequently proves more destructive and persistent than any economic sanction. News of a data breach or compliance failure erodes patient and partner trust, potentially driving away business and scaring off investors. This erosion of trust often sounds the final alarm for emerging companies, making recovery nearly impossible. In the healthcare sector, a tarnished reputation is incredibly difficult to restore.
Best practices to ensure healthcare software compliance
Achieving and maintaining healthcare software compliance requires a proactive, layered strategy integrated into every phase of the development lifecycle. It is not a feature that can be bolted on at the end, but a core principle that must guide the entire process. For teams seeking to build this competency, engaging with a specialized healthcare IT consulting service can provide the strategic direction needed to navigate such a complex landscape effectively. Now, it’s time to explore the foundational pillars of a secure development framework.
1. Privacy by design & default
Such a philosophy mandates that privacy and data protection healthcare considerations are embedded into the system architecture from the very beginning, not added later as an afterthought. It means that by default, the application should collect only the data absolutely necessary for its specified purpose, retain that information for the shortest time possible, and automatically protect it without requiring user intervention.
This approach fundamentally minimizes the data footprint and associated risk. Implementing this principle effectively often starts with healthcare UX/UI design that intuitively guides users toward secure choices and transparently communicates how their information is being leveraged.
2. DevSecOps with CI/CD testing
The traditional approach of conducting security reviews only at the end of a development cycle is obsolete. The DevSecOps methodology embeds protective measures directly into the development-operations workflow, distributing security ownership uniformly among every unit.
Enhanced CI/CD channels incorporate automated scanning utilities that examine all code modifications for potential weaknesses during each integration cycle. This allows developers to find and fix security flaws early, reducing cost and effort while significantly improving the overall safety posture of the final product.
3. Data encryption
Encryption is a non-negotiable technical control for any application handling sensitive health information. It acts as a last line of defense, ensuring that even if data is intercepted or stolen, it remains unreadable without the decryption keys.
Effective implementation requires encrypting data in two states: at rest while it is stored on servers or devices, and in transit as it moves across networks. Using strong, industry-standard algorithms is critical for rendering information useless to unauthorized parties.
4. Secure coding practices
The foundation of any resilient application is code that is written with security in mind from the first line. This necessitates educating engineering groups on secure coding methodologies to prevent widespread weaknesses such as database query manipulation, client-side script injection, and memory storage overruns.
Adhering to established secure coding standards, conducting regular peer code reviews, and using static and dynamic analysis tools are all essential measures to prevent introducing weaknesses that could be exploited later.
5. Multi-factor authentication & RBAC
Robust access control is paramount. Implementing multi-step verification introduces an essential security barrier that extends far beyond simple passwords, demanding users present multiple proofs of identity to enter systems. This approach significantly diminishes the danger of unauthorized account control resulting from compromised login details.
Working in tandem with such a method, permission-based access governance guarantees that individuals, once validated, can solely reach data and capabilities required for their particular responsibilities. A doctor, for instance, would have different permissions than a medical billing specialist, enforcing the principle of least privilege.
6. Continuous monitoring & regular testing
Security is a continuous process. Proactive monitoring of systems and networks is essential for detecting and responding to suspicious activity in real-time. Furthermore, regular penetration testing and vulnerability assessments, conducted by internal teams or third-party experts, are crucial for identifying and remediating weaknesses before malicious actors can find them.
This ongoing vigilance is supported by comprehensive healthcare software testing and application maintenance and support services. Ultimately, it creates a proactive safety posture where potential threats are neutralized before they can impact patient care or data integrity.
How to balance data security, compliance & UX in health apps
A common misconception is that stringent security inevitably leads to a poor user experience. In reality, a well-designed system seamlessly integrates protection into the user journey. The key is to make security intuitive, not intrusive. Achieving this harmony relies on several strategies:
- Secure user experience: Design intuitive flows that incorporate biometric authentication like fingerprint or face ID, offering both high safety and speed while eliminating password-related friction. More details on this in our guide to finding and fixing UX issues.
- Biometrics & adaptive MFA: Implement intelligent authentication that assesses risk contextually, requesting additional verification only for unusual login attempts such as those from new devices or locations.
- Clear privacy policies: Build trust through transparency by presenting concise, understandable privacy policies at crucial decision points, empowering users and demonstrating respect for their data.
As organizations refresh existing platforms, legacy software modernization becomes a practical way to rebuild architectures that embed security and usability in tandem.
“The most effective healthcare security feels invisible to users yet remains impenetrable to threats.”
Build secure, compliant healthcare apps with Halo Lab
At Halo Lab, we understand that creating a digital health solution that is both innovative and fully compliant presents a monumental challenge. It demands specialized expertise in cutting-edge technology and the intricate healthcare regulatory landscape. Our team brings a proven track record in this domain, helping de-risk your entire development journey.
From initial strategy and user-centric design to rigorous testing and ongoing support, we ensure that data security in healthcare and healthcare software compliance form the foundation of your application. If you need a solution that users can trust and that meets all legal obligations, just contact us.
in your mind?
Let’s communicate.

Frequently Asked Questions
What is a compliant healthcare app?
A compliant medical application is one that adheres to all relevant legal and regulatory frameworks governing the regions where it operates. This encompasses formal policies, staff training, risk assessments, and documented procedures for handling data breaches.
Do all healthcare apps need HIPAA or GDPR compliance?
Not every wellness app falls under these strict regulations. The applicability depends on the app’s functionality and the data it handles. If an application is created by or for a covered entity like a hospital or insurer and transmits identifiable health information, HIPAA likely applies. GDPR has a broader scope, impacting any app that processes the personal data of individuals in the EU.
How can patients know if an app is safe?
Users should look for clear and accessible privacy policies that explain how their data is collected, leveraged, and shared. Reputable apps often publicly state their compliance with standards like HIPAA or display certifications.
Can small startups meet healthcare compliance requirements?
Absolutely. While challenging, it is entirely feasible for startups to achieve compliance. A focused approach that prioritizes security from the outset can make the process manageable and cost-effective.
Is it possible to comply with multiple regulations at once?
Yes, and it is a common practice for apps with international ambitions. Many core principles of data protection in healthcare are universal.
How long does it take to get a healthcare app audited?
The timeline for a compliance audit can vary significantly based on the app’s complexity, the scope of the audit, and the specific regulatory standard. A preliminary internal assessment might take a few weeks, while a full formal certification like ISO 27001 can be a project spanning several months.




















.webp)