Transforming an idea into a dependable, compliant, and scalable product in the intricate environment of health IT involves structured validation. Whether you’re building a telemedicine app, an AI diagnostic assistant, or an EHR integration tool, the most important decision you’ll make early on is proof of concept (PoC) vs prototype, which should be built first?
The initial experimental stage tests an idea to demonstrate its technical viability, while a preliminary model helps build and visualize the user experience. Both are critical phases to creating software for healthcare, and knowing when and how to do it can save you months of time and millions of dollars. To better understand the landscape in which the mentioned validation methods are applied, you can explore our article on healthcare software types.
Navigating the earliest stages of a digital project requires a clear strategy for confirming feasibility. This piece compares two foundational approaches, providing a framework to determine the right path for your initiative.
Why early validation matters in healthcare IT
Early verification is key to any success in medical innovation. Strict regulatory constraints, interoperability concerns, and high standards for safety and usability make initial confirmation critical to avoiding the derailment of even the strongest concepts.

Checking and iterating on design during formative stages allows healthcare companies to avert expensive rework and can protect patient outcomes. Organizations aiming to enhance an interface or workflow can always consider utilizing our UI/UX design services for support.
“A disciplined, upfront verification process bridges the critical gap between a promising concept and a deployable, trustworthy clinical tool.” {{sergiy-s.}}
What is a proof of concept (PoC) in healthcare IT?
An initial technical trial is a first experiment set up to demonstrate that a new concept technically and operationally works as a solution. This raises the question: can such an approach be effective, in practice, under the constraints imposed by medical technology and regulation?
A PoC in healthcare IT will typically have a limited set of features or dataset/s to study, but assess the viability of key functionality, security, & compliance. For example, a developer might leverage this method to check if an AI model was able to read ECG records or check if an EHR integration was sufficiently proficient to meet interoperability criteria. For a full overview, check out our blog post on PoC in software development.
Benefits of a proof of concept for healthcare IT projects
This approach serves as the first checkpoint in validating innovations. It helps teams test ideas in controlled conditions before scaling, ensuring the solution is technically sound and also compliant and practical for real-world use. Now, let’s talk about that in more detail:
- Technical feasibility and integration checks
A PoC confirms that your concept can function within the complex architecture of healthcare systems. It validates whether APIs, databases, and hospital IT environments can handle new integrations without compromising performance or data security. For example, testing FHIR (Fast Healthcare Interoperability Resources) integration in this phase helps identify issues with data exchange formats or latency before full-scale EHR rollout, preventing costly redevelopment later.
- Regulatory preparedness (HIPAA, GDPR, FDA, MDR)
Healthcare compliance is multifaceted, and overlooking early regulatory risks can stall an entire project. A PoC allows teams to evaluate whether their concept meets HIPAA standards for patient data encryption or if data residency under GDPR could conflict with cloud storage plans. For instance, this approach might reveal that anonymized datasets used in an AI model still contain identifiable metadata, helping teams correct issues before clinical testing. Similarly, for FDA-regulated devices, the PoC phase can expose documentation gaps that would otherwise delay certification.

- Early stakeholder confidence
Demonstrating a working proof of concept gives stakeholders more than theory; it provides evidence that the idea can translate into a safe, functional healthcare solution. Clinical partners and hospital boards often respond positively to PoCs because they can see early data, usability insights, and technical validation before committing budget or operational resources. Investors, too, are more inclined to support projects with measurable proof, as in this case, their outcomes reduce uncertainty and highlight tangible progress toward implementation.
- Risk mitigation
Healthcare projects involve high stakes both financially and ethically. A PoC minimizes these risks by identifying vulnerabilities before full deployment. For example, testing device connectivity in a hospital network may uncover bandwidth or firewall issues; validating an AI diagnostic algorithm may reveal bias or underperformance with specific demographic data. By catching such problems early, organizations prevent large-scale failures, safeguard patient safety, and ensure compliance throughout the development lifecycle.
- Resource optimization
A PoC enables healthcare organizations to manage technical, financial, and human resources more effectively. It helps allocate skilled personnel, developers, clinicians, and data scientists to initiatives that have proven potential, while deprioritizing those that don’t meet feasibility benchmarks. For example, if it turned out that integrating a new wearable device with existing EHRs demands excessive manual configuration, resources can be redirected to automation or interface redesign instead of being wasted on full-scale deployment. In short, this approach outcomes guide smarter budgeting, workload planning, and technical investments.
What is a prototype in healthcare IT?
A preliminary version is a tangible, interactive representation of a product that simulates its design, functionality, and user experience. While a PoC answers “Can it work?”, a prototype addresses “How will it look, feel, and perform for real users?”
Healthcare functional mock-ups help designers and stakeholders visualize patient dashboards, clinical workflows, and app interactions before writing production-level code. They serve as essential tools for feedback, testing, and iteration.
For more insight, explore our following articles: What is a UX prototype in design, and Prototype vs MVP: how they differ.
Types of prototypes in healthcare IT
Prototyping isn’t one-size-fits-all. Each type serves a unique purpose, whether to explore early design ideas, test functionality, or simulate a near-final experience for clinical validation. Understanding these distinctions helps teams choose the right level of fidelity at the right time.
- Low-fidelity prototype
The mentioned category includes quick, paper-based, or wireframe mockups that represent layout and navigation. In healthcare, they’re often used to sketch patient intake flows, EHR dashboard layouts, or appointment scheduling sequences before any visual design begins. It is an ideal choice for brainstorming workflows with clinicians or testing basic screen logic early on.
- High-fidelity prototype
These models look and feel close to the final product, including visuals, typography, and branding. They’re commonly employed in healthcare for stakeholder presentations or UX validation of clinical applications such as medication management dashboards or teleconsultation interfaces, where realistic visuals help test usability and trust perception among medical professionals.
- Functional prototype
Such a version mimics real functionality, buttons, data entry, or limited backend features. In healthcare IT, functional prototypes help simulate data entry forms, lab result visualizations, or AI-driven alerts to verify that the workflow aligns with clinicians’ real tasks and regulatory data handling.
- Visual prototype
A non-interactive design that communicates brand tone, color, and style guidelines for future development. These are especially valuable for patient-facing portals or mobile wellness apps, where the aesthetic and emotional tone must convey empathy, trust, and accessibility.
- Rapid prototype
Quick iterations are built to gather fast feedback. In healthcare settings, rapid prototyping often uses tools like Figma, Adobe XD, or InVision, combined with short testing cycles (2–5 days) involving doctors, nurses, or patients. Such prototypes evolve rapidly, testing concepts such as triage interfaces, vital sign dashboards, or remote monitoring controls.

Benefits of a prototype for healthcare projects
The advantages of employing a preliminary model extend far beyond simple visualization. In the high-stakes environment of healthcare, such an approach delivers concrete, multifaceted benefits that are critical for both clinical efficacy and user adoption. Now, let’s take a closer look at these strengths:
- Usability testing and UX validation
Prototypes let real users, clinicians, nurses, and patients interact with flows before any code is shipped. Observing task success, time-on-task, and error rates reveals where confusion or cognitive load is highest. Fixing those issues at the prototype stage prevents safety risks and costly rework later. See our healthcare software testing services for structured usability protocols.
- Visualizing the product
High-fidelity prototypes make the future tangible for executives, IT, and clinical leadership. When stakeholders can see appointment flows, alert states, and data visualizations, they align faster on scope and priorities, often accelerating funding and governance approvals.
- Early detection of design flaws
Clickable models expose gaps in navigation, readability, and information hierarchy that static screens hide. For example, a medication-ordering prototype may surface that dosage fields need guardrails or that critical warnings require stronger visual prominence, preventing downstream clinical risk.
- Optimizing сlinical workflows
Iterative modeling lets teams map real clinician behavior (handoffs, interruptions, parallel tasks) to interface logic. By testing variations of order sets, lab-result drill-downs, or note templates, you can shorten the path-to-action and reduce clicks directly, improving throughput and reducing burnout.
- Improving patient engagement
Patient-facing prototypes allow UX teams to check what actually drives adherence from reminder frequency and tone, to dashboard clarity, to micro-interactions that reward progress. When patients immediately see trend lines (e.g., BP or glucose), receive timely nudges, and can message care teams without friction, this testing typically shows higher return rates and completed tasks, which translate to better outcomes.
Proof of concept vs prototype: key differences
While both PoCs and prototypes validate ideas, they serve different goals. In healthcare, the difference between two approaches often lies in purpose, depth, and target audience. Further information is provided in the table below.
For more insights, visit our healthcare and medical web design services.
PoC vs prototype: choosing the right approach for your project
Selecting between methods depends on your project’s maturity, risk level, and business objectives. In many healthcare IT initiatives, both are necessary, but they occur in sequence. For expert guidance, explore our healthcare IT services, and here’s a more detailed look at the approaches.
Proof of concept
- AI for ECG analysis
A PoC can test whether an AI model can reliably detect cardiac arrhythmias from anonymized ECG datasets. For instance, a data science team might use 10,000 de-identified ECG samples from a partner hospital to train and validate the algorithm. This approach helps confirm accuracy rates and also whether the AI integrates with existing EHR systems for real-time clinical alerts, a vital step before regulatory review.
- EHR integration PoC
Prior to investing in a full rollout, teams can run a small-scale pilot to test data exchange between a new clinical app and established EHR platforms like Epic or Cerner. For example, a PoC might focus on syncing medication orders or lab results from one module to the main EHR in compliance with FHIR standards. The results reveal interoperability challenges, permission conflicts, and latency issues that inform a safer, scalable integration plan.
- IoT-enabled medical devices
A PoC for connected devices (e.g., glucose monitors or heart-rate sensors) can validate secure data transmission and latency under hospital Wi-Fi conditions. Developers might set up 20 devices in a single ward to measure signal consistency and battery performance during clinical rounds. Insights from this phase often guide firmware updates, network configurations, and cybersecurity protocols before commercial launch.

Prototype
- Telemedicine dashboard
Once a PoC confirms video reliability and HIPAA-secure transmission, a prototype refines how clinicians manage patient sessions. For instance, UX designers may simulate the scheduling interface, in-call controls, and follow-up notes while observing physicians during mock consultations. Feedback on layout, click reduction, and alert timing helps optimize session flow and reduce physician fatigue.
- Mobile health app
User-centered prototyping helps shape intuitive navigation for patients managing chronic conditions. Designers might test a medication reminder flow with actual patients, observing completion rates and comprehension of alerts. These insights inform adjustments to color cues, reminder frequency, or tone of messages, ensuring accessibility for older adults or users with low digital literacy. To examine how such principles are applied in real-world projects, explore our healthcare app development services and mobile app design process guide.
- AI diagnostic interface
High-fidelity prototypes visualize how clinicians interact with AI-generated insights within existing workflows. A design team might mock up an oncology dashboard that displays tumor-detection confidence scores alongside CT images. Usability testing ensures results are displayed in a way that complements, not overwhelms, clinical decision-making and aligns with FDA expectations for explainable AI outputs.
- EHR integration prototype
When connecting new modules to an EHR, prototypes test workflow alignment, data visibility, and user permissions before production coding. For example, an interactive mock-up could simulate how a physician retrieves lab reports or enters discharge summaries through a third-party module. Early testing may reveal navigation redundancies or compliance gaps in audit logging, allowing teams to refine before full-scale integration.
- Patient monitoring portal
Interactive prototypes help fine-tune dashboards for remote patient monitoring programs. Designers might test alert prioritization, color coding, and notification thresholds with clinicians to ensure that critical vitals stand out while minimizing alarm fatigue. Patients, in turn, can test simplified trend views or daily check-in forms to confirm usability on mobile devices, improving both engagement and data accuracy.
Common pitfalls when using PoC and prototype
Even experienced teams can stumble when handling early validation stages. Common mistakes include:
- Skipping validation stages
Rushing straight into full-scale development without confirming feasibility or usability can backfire. For example, a startup might build an AI symptom checker before verifying its medical content accuracy or data sources, leading to misinformation and compliance risks.
- Over-engineering early versions
Teams sometimes add advanced features, such as AI predictions, multi-language support, or integration modules, before proving the product’s core workflow. A telehealth platform that builds complex analytics dashboards before stabilizing its video connection is a classic case of over-engineering too soon.
- Ignoring user and clinical feedback
Designing without input from real clinicians or patients often results in tools that look great but don’t fit daily routines. For instance, an EHR prototype that ignores nurse feedback on patient charting shortcuts may slow documentation rather than improve it, hurting adoption rates.
- Neglecting compliance early
Skipping early HIPAA or GDPR reviews can expose projects to massive redesigns later. A PoC that doesn’t encrypt patient test results or log access events might pass internal testing but fail regulatory audits — delaying launch and increasing cost.
- Lack of measurable goals
Without clear success metrics, teams struggle to evaluate progress or justify investment. For example, a hospital innovation lab may complete a PoC for a mobile triage tool but fail to define KPIs like response time reduction or clinician satisfaction, making it impossible to prove ROI.
How to avoid these pitfalls? Structured milestones, early clinician involvement, measurable KPIs, and proactive compliance checks can help teams validate faster, reduce risk, and ensure their healthcare innovations are both effective and audit-ready.
“In healthcare IT, speed without validation is risk disguised as progress.” {{sergiy-s.}}
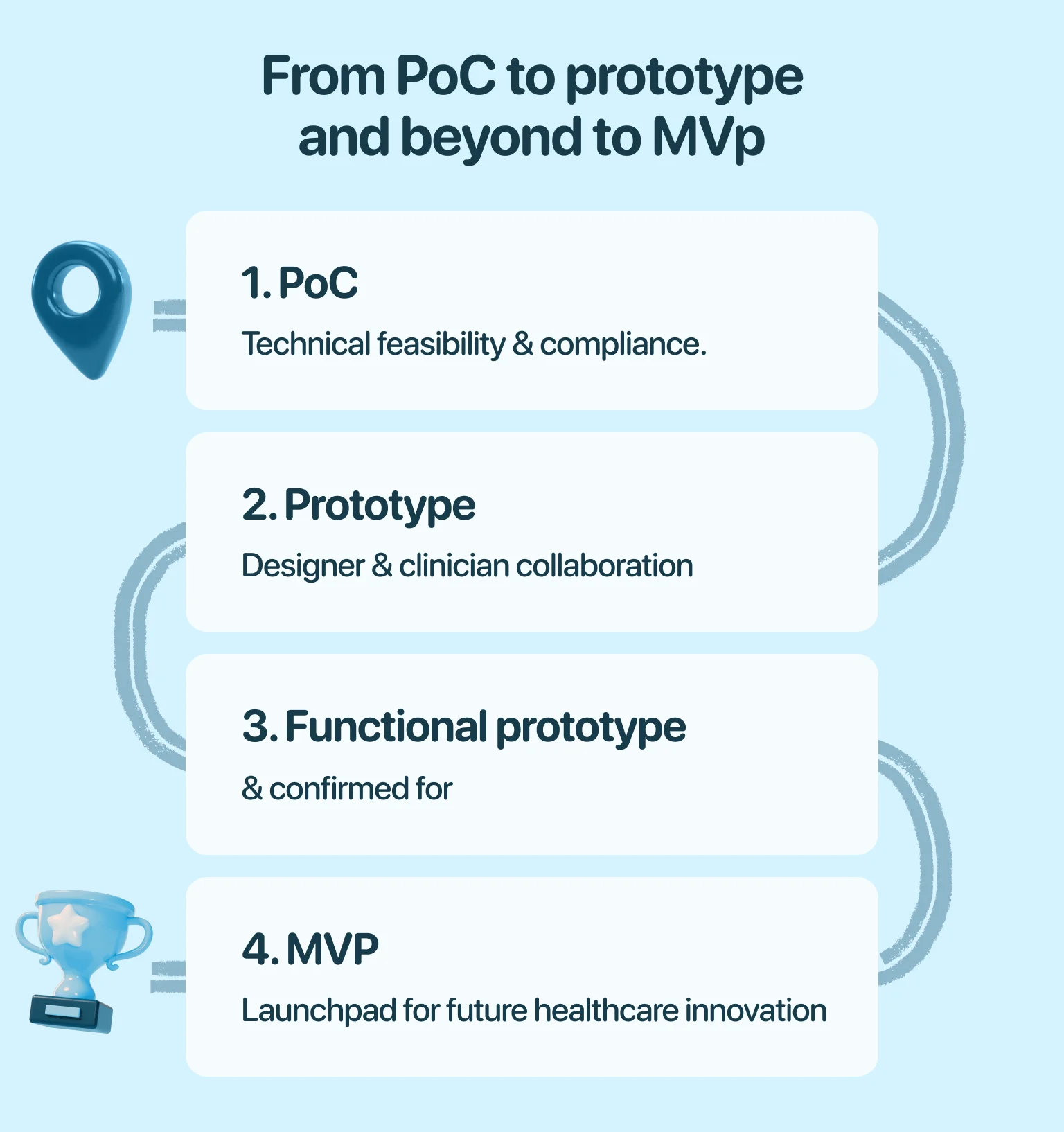
From proof of concept to prototype and beyond to MVP
Every healthcare innovation starts as a hypothesis, an idea that promises to improve patient outcomes, streamline workflows, or make data more actionable. The journey from PoC to prototype to minimum viable product (MVP) transforms that idea into a validated, real-world solution through structured evolution.
It begins with the PoC, where teams focus on verifying technical feasibility and compliance. This stage asks a fundamental question: Can this work in a healthcare environment? By testing a limited dataset or integration with hospital systems, the method identifies technical risks, regulatory constraints, and foundational requirements for success. Once feasibility and compliance are confirmed, attention shifts toward usability.
The prototype stage translates those technical findings into tangible user experiences. Designers and clinicians collaborate to define how the product will look, behave, and support clinical tasks. At this point, workflows are refined through interactive models from physician dashboards to patient-facing portals, ensuring the solution is intuitive, accessible, and compliant before any production code is written.
Finally, the MVP brings together the validated technology and tested user experience into a functional product ready for real-world deployment. It contains only the essential features necessary to demonstrate value, collect user feedback, and measure clinical or operational impact. Successful MVPs form the launchpad for future iterations, backed by data from actual users and environments.
In essence, the transition from PoC to prototype to MVP is a process of de-risking innovation at each stage, narrowing uncertainty, improving design, and building confidence until a healthcare idea becomes a viable, market-ready solution. This staged approach ensures safety, scalability, and user satisfaction, three pillars of healthcare innovation. To take your concept through these stages, explore Halo Lab’s MVP development services.
Ready to turn your healthcare IT idea into a validated solution?
Building healthcare software isn’t just about code, it’s about trust, accuracy, and patient outcomes. Partnering with the right design and development team can turn an idea into a clinically relevant, regulatory-compliant, and user-approved product.
If you’re ready to validate your concept and bring it to life, discover Halo Lab’s healthcare IT services and start your journey from the PoC to a market-ready solution.
in your mind?
Let’s communicate.

Frequently Asked Questions
How long does a PoC typically take in healthcare IT projects?
Most PoCs take 4–8 weeks, depending on complexity. AI or EHR integration PoCs may require additional time for data access and compliance reviews.
Can a prototype be developed without a proof of concept first?
Yes, if the technology is already proven. However, for innovative or regulatory-heavy ideas, skipping the PoC can increase technical and compliance risks.
Can small startups run a PoC or prototype without a large team?
Absolutely. Lean development methods and cloud-based testing environments make it possible for small teams to validate ideas efficiently.
How long does it usually take to build a prototype?
A low-fidelity prototype can take a few days, while a high-fidelity interactive model may take 3–6 weeks, depending on features and user testing needs.
How do PoCs and prototypes impact project costs?
Both save money long-term by preventing costly rework. A PoC validates feasibility, and a prototype prevents usability issues. Together, they reduce total project risk.
Should patients be involved in prototype testing?
Yes. Involving patients ensures accessibility and empathy-driven design, leading to higher engagement and adoption rates.




















.webp)